“PTSD is a whole-body tragedy, an integral human event of enormous proportions with massive repercussions.” ~ Susan Pease Banitt, The Trauma Tool Kit: Healing PTSD from the Inside Out Addiction is a disease with several causal factors – genetics, environment, personal behavior, and experience, in the form of trauma. The relationship between trauma and substance abuse is complicated and closely intertwined. In other words, the road between the two goes both ways, and the negative consequences of one disorder can worsen the problems of the other. 
What Is Meant by “Trauma”?
In psychological terms, trauma is a situation or an event that a person simply cannot cope with. It can leave the person in an extreme state of fear, making them overwhelmingly afraid of imminent death, destruction, or actual physical or mental harm. A person who has suffered trauma first-hand will experience an entire list of negative emotions:
- helplessness
- confusion
- betrayal
- pain
- entrapment
- powerlessness
- confusion
- loss
- terror
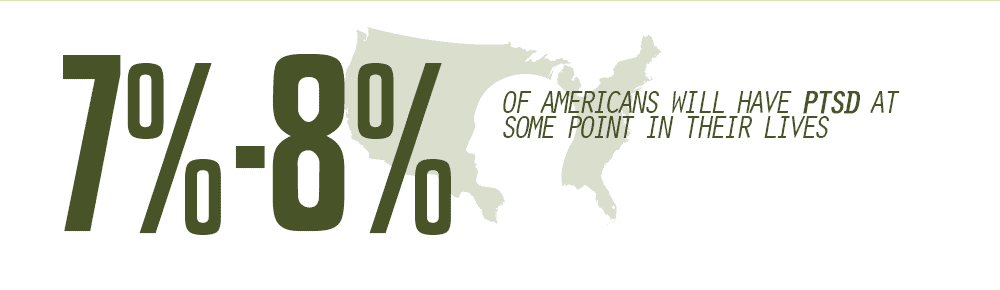
Most of those emotions are temporary. However, a person who has suffered a sufficiently traumatic event can experience post-traumatic stress disorder (PTSD). PTSD can manifest at any time and can last for years and even a lifetime. In the United States a significant portion of the population has diagnosable PTSD at any given time:
- 7%-8% of Americans will have PTSD at some point in their lives
- Women suffer from PTSD at higher lifetime rates – 10%, versus 4% for men
- In any given year, 8 million US adults will have PTSD
What Causes Trauma?
Trauma is a very personal experience that depends upon the individual. It can be a response to a single, one-time occurrence, or it can be developed over time because of a chronic or systematic situation. Some of the causes of trauma might include –
- child abuse
- neglect
- violence
- bullying
- accidents
- crime
- natural disasters
- domestic assault
- extreme deprivation
- sexual assault
- war
What is important to note is that a person who suffers from an exposure to trauma doesn’t necessarily need to be the victim – witnessing any of these occurrences can be sufficiently harmful.
How Prevalent Is Trauma Exposure?
When a person’s entire lifetime is considered, the possibility of exposure to trauma is much higher than might be imagined –
- up to 25% of women will experience sexual abuse
- domestic violence can affect as much as 44% of American women
- 18.5% of veterans suffer from PTSD or depression
- 18.9% of men and 15.2% of women will experience a natural disaster
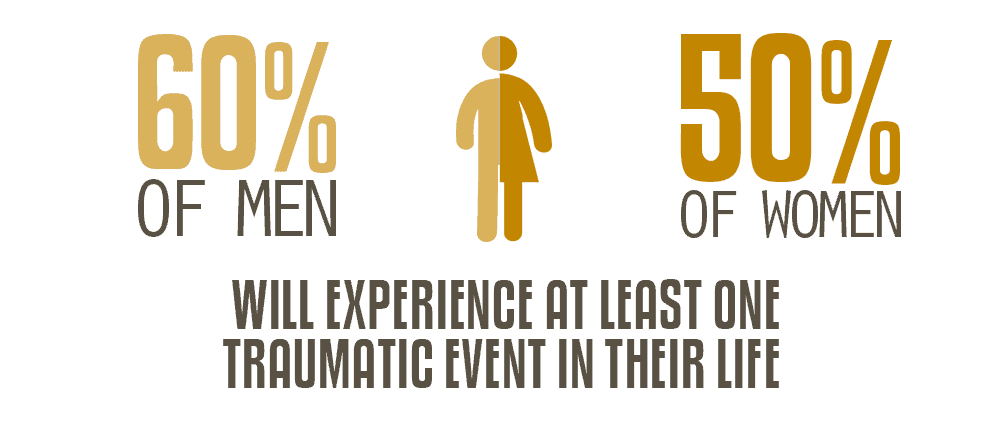
According to the National Center for PTSD, approximate 60% of men and 50% of women will experience at least one traumatic event in their life. Almost three-fourths of individuals who receive treatment for substance abuse also have a history of exposure to trauma. Conversely, individuals who have suffered assault or sexual abuse are three times as likely to abuse drugs and/or alcohol.
Trauma Increases the Likelihood of Substance Abuse
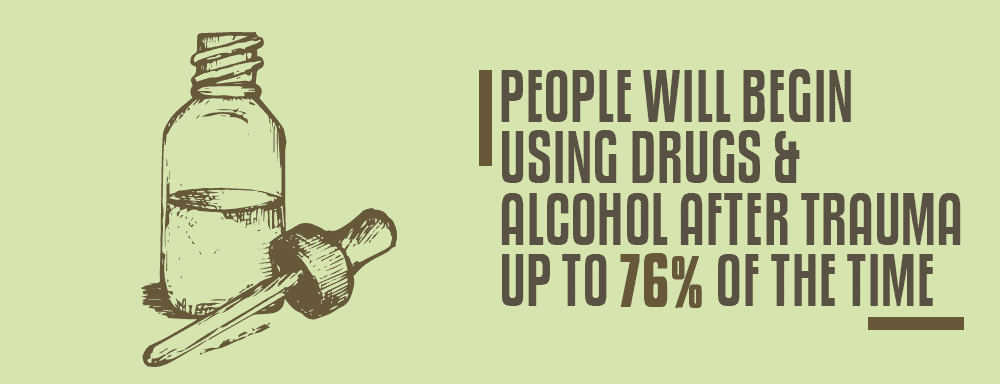
On the one hand, a person experiencing a trauma is at greater risk for drug and/or alcohol abuse. People turn to intoxicating or illicit substances in times list substances in an attempt to “self-medicate”, as they try to deal with the negative emotions and symptoms associated with PTSD. According to the National Child Traumatic Stress Network, a person will begin using drugs and alcohol after experiencing a trauma up to 76% of the time. Up to 59% of people with PTSD will develop a problem with alcohol and/or drugs. Post-traumatic stress disorder can also make it harder for an individual to stop drinking or using drugs, because any reminders of the trauma can trigger cravings.
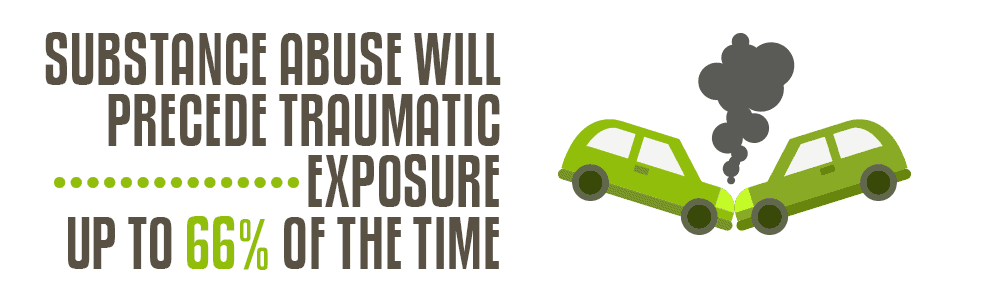
Substance Abuse Increases the Likelihood of Trauma
Conversely, substance abuse will precede traumatic exposure up to 66% of the time. This direct link is because alcohol and drug use leads people to engage in risky behavior that may result in injury to themselves or others –
- driving under the influence
- fighting
- placing themselves in dangerous situations
- unsafe sexual behavior
- increased risk-taking
- self-harm
Substance Abuse Interferes with Recovery from Trauma
Because of the cognitive, psycho-social, and behavioral impairment associated with long-term alcoholism and drug addiction, individuals with substance abuse disorders are often unable to properly cope after experiencing a traumatic event. For example, adolescents who abuse alcohol and/or drugs are twice as likely to experience symptoms of PTSD following a traumatic event then their peers who use neither. In fact, their method of coping – self-medicating with drugs and alcohol – only exacerbates the problem. When a person has a traumatic experience and substance abuse is their coping mechanism, they may initially feel better, due to two factors:
- drugs and alcohol activate the brain’s reward centers, so the abuser will enjoy temporary pleasurable sensations
- people who abuse alcohol and/or drugs “mask” their negative emotions, so they never have to fully experience and process them
Neither of these means of coping is “real”, so recovery from the trauma never actually happens.
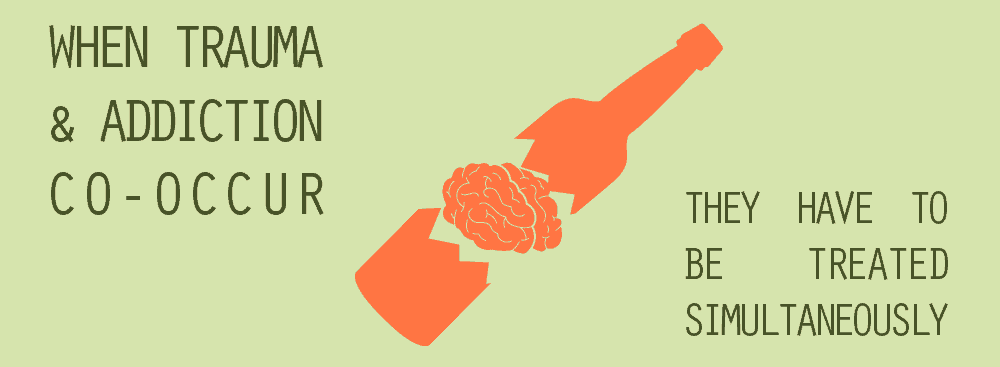
When PTSD and Substance Abuse Co-Occur
It is obvious that the two disorders can overlap, but it is less obvious to the inattentive or untrained eye when that actually occurs. When dealing with a patient with PTSD, mental health professionals in a clinical setting may not have the opportunity to observe any symptoms of substance abuse. At the same time, addiction specialists in a drug rehabilitation facility may concentrate so much on the treatment of addiction that they miss the co-occurring PTSD. This is the challenge of successful recovery. Because the two disorders feed off of each other, when they are not both treated simultaneously, the treatment for the one invariably fails.
How Addiction and PTSD (Major Trauma) Can Be Successfully Treated
The best addiction treatment facilities have trained and experienced staff members who understand that when there is a tool diagnosis of PTSD and substance abuse disorder, there needs to be a multilevel approach to treatment.
- Individual therapy – so the recovering addict/alcoholic can learn to identify those triggers that can lead to cravings and relapse.
- Group sessions – so the common problems and challenges faced by people with both a substance abuse disorder and PTSD can be addressed communally
- Family and couples counseling – to educate family members about the dual disorders and to rebuild/strengthen familial relationships.
- 12-Step meetings – so the recovering addict/alcoholic can draw strength and inspiration from the common experiences and fellowship of others
- Medication-based therapy – with a combination of anti-addiction drugs, antidepressants, and/or anti-anxiety medicines
A person who is dealing with both PTSD because of a past traumatic event and an addiction to drugs and/or alcohol can get better if they participate in the right substance abuse rehabilitation program – one that specializes in the treatment of individuals with a dual diagnosis. When both disorders are addressed, the chances of a successful recovery are greatly increased.
What Did you Think About This Blog?
Give it a Rating!