In the world of addiction treatment, there will always be differing opinions about the best way to help chronic substance abusers get clean and sober, and just as importantly, stay that way by achieving long-term recovery.
The Need Has Never Been Greater
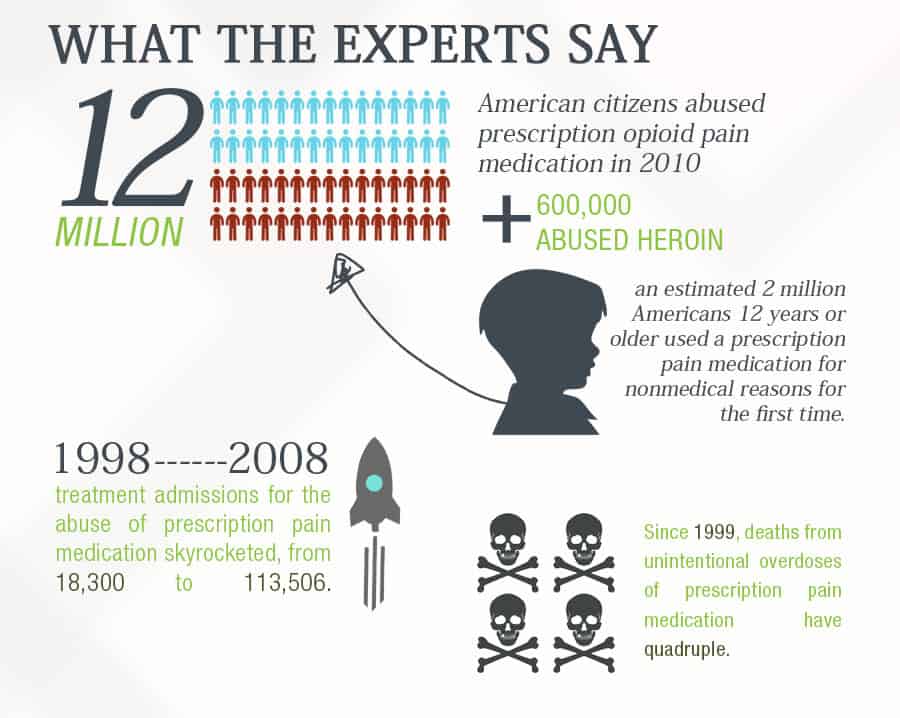
Opioid addiction has reached near-crisis levels in the United States. Consider these statistics disseminated by The National Survey on Drug Use and Health, put out by the Substance Abuse and Mental Health Services Administration:
- In 2010, approximately 12 million American citizens abused prescription opioid pain medication, and an additional 600,000-plus abused heroin.
- Also in 2010, an estimated 2 million Americans 12 years or older used prescription pain medication for nonmedical reasons for the first time. That rate for first-time use was second only to marijuana.
- In the 10 year period, 1998-2008, treatment admissions for the abuse of prescription pain medication skyrocketed, from 18,300 to 113,506.
- Since 1999, deaths from unintentional overdoses of prescription pain medication have quadrupled.
There Is a Solution, but How to Use It?
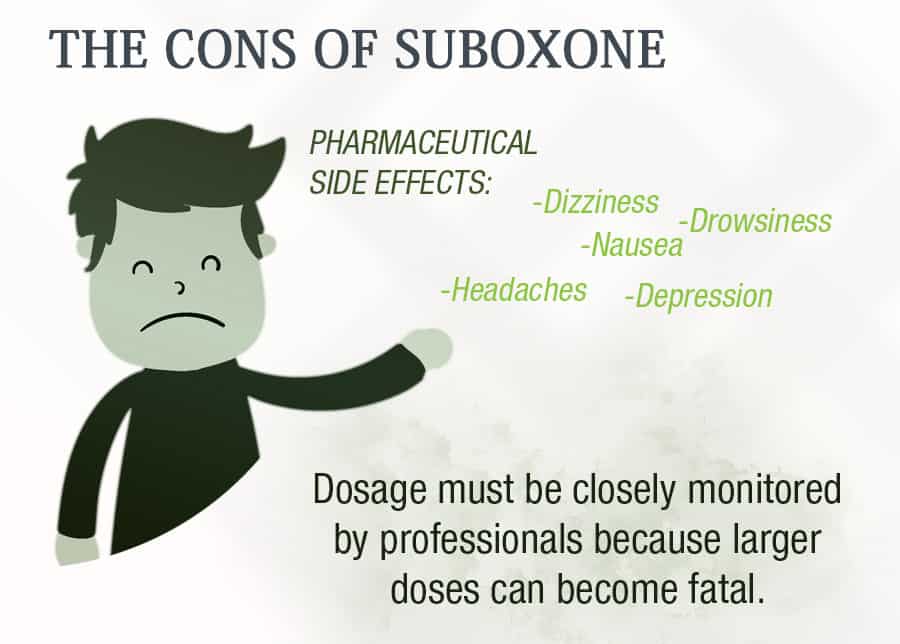
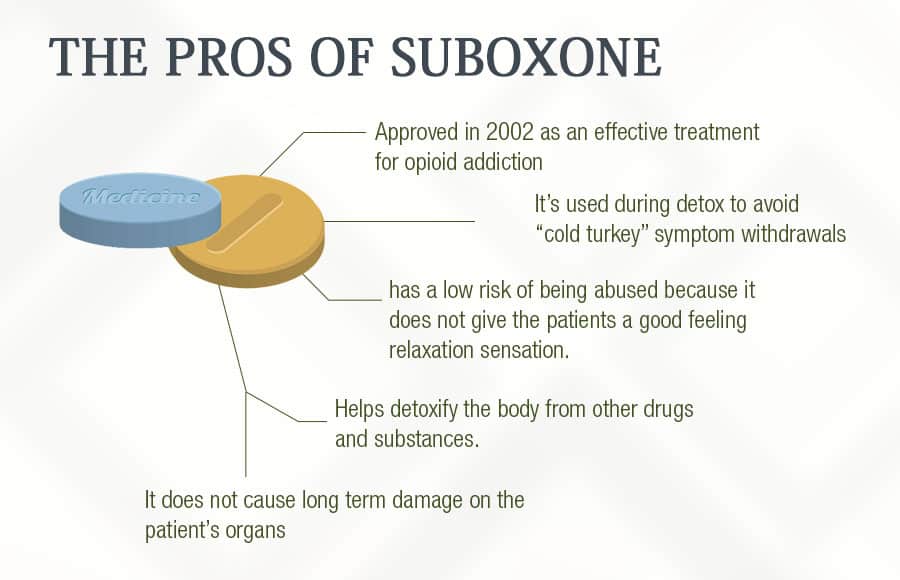
In Boise, Idaho, as it is elsewhere throughout the country, one of the points of contention is how to properly treat opioid addiction with the drug buprenorphine, commonly known as Suboxone. Suboxone binds to the brain’s opioid receptor, which is the same area where heroin, morphine, and other opiates bind. Suboxone is so uniquely valuable and opioid detox/addiction treatment because it is known as a “partial agonist”. What this means is that at lower doses, Suboxone suppresses pain, just like any other opiates. However, that increased dosages, it starts blocking the opioid receptor from receiving any more stimulation. This allows medical personnel to ease an addict’s withdrawal symptoms without fear that the patient will start abusing Suboxone. Best of all, because the body’s opioid receptor is blocked, it is no longer possible for the addict to get high on other opiates. So, if a person who is taking their prescribed Suboxone uses OxyContin or heroin, for example, they will not feel their customary euphoric rush. The key issue seems to be whether Suboxone should be used during detox to ease withdrawal symptoms – short-term only – or whether it should be administered long-term as a means to help the recovering opioid addict abstain from relapsing. Let’s take a look at both sides of the argument.
“We treat opioid addiction and accept many health insurance plans. Take a look at our program.”
Suboxone During Detox
“When patients receive buprenorphine instead of clonidine to help them with opioid withdrawal, they are more likely to succeed. Study outcomes from the CTN in have shown this success in both inpatient and outpatient settings. Significantly more in patients assigned to buprenorphine (77%) completed the 13-day taper program and provided opioid-negative urine samples than those assigned to clonidine.” ~ Blending Initiative NIDA/SAMHSA, Short-Term Opioid Withdrawal Using Buprenorphine: Findings and Strategies from a NIDA Clinical Trials Network (CTN) Study
Suboxone is so important during Suboxone detox, because once an opiate abuser ceases using “cold turkey”, they will begin experiencing withdrawal symptoms within a few short hours:
- excessive sweating
- racing heartbeat
- nausea
- muscle pain
- insomnia
- extreme anxiety
Typically, an individual new to recovery will have taken the last dose of their drug of choice shortly before entering the drug detox facility. Immediately, the detox staff will begin monitoring the patient for the onset of mild withdrawal symptoms, and once they have presented, begin administering Suboxone. Interestingly, even though Suboxone will suppress withdrawal symptoms, easing them virtually completely in as few as 4 to 6 hours, clinicians are extremely careful to not give the medication until symptoms manifest. Given too early, Suboxone can actually trigger withdrawal symptoms precipitously. Typically, a detoxing opiate addict on a medication-assisted program using Suboxone will need to have the drug administered for three or four days. The most chronic abusers might need additional time, usually no more than two weeks. It is important to note that Suboxone is typically used during detox only for the management of opioid withdrawal symptoms. If the individual has been an abuser of other substances, such as Valium, marijuana, alcohol, cocaine, etc., other medications may be necessary. Also, recovering opioid addicts are often prescribed and anxiety or sleeping medications or muscle relaxants because of spasms or muscle pain.
Long-Term Suboxone Maintenance
“Buprenorphine is the most important advance, certainly in heroin and opiate treatment, if not all addiction treatments in the last 30 years.”~ Dr. Alan Leshner, former Director of the National Institutes of Drug Abuse, speaking to the New York Times
Those who argue that Suboxone should be used for long-term maintenance to suppress cravings say that, while not perfect, is an acceptable solution for the “typical” addict’s life – crime, chronic unemployment, inescapable poverty, and the desperate actions of a drug-seeker. Also, even though the individual has to continually take the medication to keep cravings tolerable, Suboxone’s properties as a partial agonist mean that it will not trigger respiratory depression – the chief contributing factor to fatal overdoses from other opiates. There is an existing treatment model specifically for those addicts who have a long history of heavy opioid abuse. When Suboxone is used as maintenance, patients are kept on the drug for months – or even years – while their addiction-damaged brain chemistry slowly heals. Because of how easy it would be for some physicians to indiscriminately place their patients on a Suboxone maintenance program, federal law has created a limit for each doctor at 100 such clients. Even still, there is almost always an extensive waiting list.
The Argument for “Detox Only” Suboxone
“I’ve seen what long-term Suboxone does. People come in with endocrine problems – thyroid dysfunction, low testosterone… hair loss – tooth loss with Suboxone. There’s no way your brain chemistry can heal why on buprenorphine. You’re continuing to give someone a narcotic.” ~ Dr. Steven Scanlan, a psychiatrist/addiction specialist who is the Medical Director of Palm Beach Outpatient Detox
The proponents of administering Suboxone only during detox argue that the true goal of recovery is for the individual to live a completely drug-free life. Making a switch from one opiate – heroin, for example – to another – Suboxone – does not allow the individual to fully recover from the neurological component of addiction. As long as either the opiate is abused or the Suboxone is administered, the body continues to decrease its endorphin production and increase the number of opioid receptors. This is the very definition of an addict’s tolerance. In other words, even though Suboxone has been approved for maintenance treatment, staying on the medication long-term after being stabilized defeats the purpose of individual sobriety.
What Did you Think About This Blog?
Give it a Rating!