The question surrounding suboxone is a simple one: Is it a good idea to treat opioid addiction with another opioid? Opioid abuse is well-known as a scourge across the country by those addicted to them, as well as police, doctors, rehab facilities, and even the federal government. It’s a public health emergency that kills tens of thousands of people each year, and appears to only be getting worse. Of course, because opioid abuse has become such a major problem, there is, obviously, a number of counter-strategies to help fight this epidemic. While behavioral therapy and counseling are always an important step to fully releasing yourself from the grip of addiction, opioids are a highly addictive substance that aren’t usually willing to let you go that easily. Identifying the root causes of your addiction aren’t going to help you beat it if your brain is still screaming at you relentlessly to take another dose. The withdrawal symptoms of opioids are often severe enough to send people right back into use without proper treatment. Luckily, there is a treatment specifically made for recovering opioid addicts. That treatment is suboxone, a synthetic opioid that works as a moderate-strength painkiller just as other prescription drugs do. But while it technically works similarly to other opioid painkillers, suboxone is most frequently used as a treatment for opioid addiction and abuse. Suboxone is generally administered during opioid detox as a sort of “step-down” drug. It hits the same parts of the brain affected by stronger opioids like heroin or OxyContin, but offers a much weaker high while also diminishing withdrawal effects. Sounds like a miracle drug, right? Well, not exactly. Suboxone helps a lot of people ween themselves off of more dangerous opioids, but it comes with its own problems. 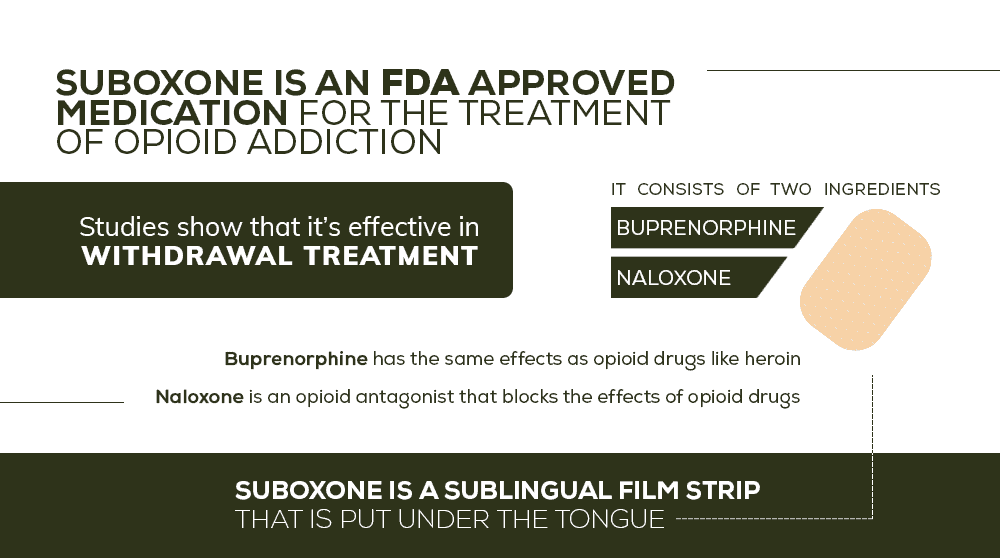
How Suboxone Works to Lessen Opioid Addiction Symptoms
Suboxone is a drug that combines two different substances: buprenorphine and naloxone. These are substances that both affect the brain, but in opposing ways. Buprenorphine is a partial opioid agonist, which means it activates the brain in the areas that opioids do – namely, the reward receptors. They don’t activate as strongly as a full opioid agonist like heroin; it provides a much duller and diminished response to the brain, which keeps withdrawal symptoms at bay during treatment. Naloxone is an opioid antagonist, which blocks the receptors in your brain that respond to opioids, and even works to flush out some of the lingering effects from opioid use. Naloxone is a useful drug for reversing the effects of opioid abuse, but when administered by itself, it can cause severe withdrawal symptoms, especially for somebody in the early stages of recovery. Suboxone combines these two drugs in a way that both satisfies the brain’s opioid receptors and begins to heal them. By doing so, it minimizes withdrawal symptoms associated with quitting opioids “cold turkey,” while also having a minimal effect on your mental state. It has, undeniably, been a breakthrough in the field of addiction treatment and has made a lot of peoples’ lives better.
“We treat opioid addiction and accept many health insurance plans. Take a look at our program.”
Suboxone is not, however, a full cure for opioid addiction. It helps with the opioid part, but addiction is a disease that affects the brain in compulsive ways. No drug can completely alter the way you think. That’s why the best use of suboxone is as a stepping stone that keeps you sober enough to be receptive to behavioral therapy and holistic addiction treatment. This is the real end goal of suboxone, is a short-term fix to make long-term treatment easier to adapt to. This approach has worked across the country, as opioid addicts who go through rehab with suboxone have better recovery rates than those who don’t. Perhaps more importantly, since Buprenorphine is technically an opioid agonist itself, it has the potential to be abused the same as any other opioid. Adding naloxone to the drug makes it much more difficult to isolate the specific opioid agonist and abuse it to satisfy addiction cravings. This is especially important considering Buprenorphine is often the subject of overdoses. Since the standard dose provides a more subtle high, abusers will take much larger amounts than they should to get the rush they’re looking for. Suboxone lowers the risk of this sort of abuse because of its naloxone component. 
The Immediate Effects of Suboxone
No matter how helpful it is, there’s no way to get around the simple truth of suboxone treatment: people who come in with an opioid addiction and leave with a prescription for suboxone? They’re still addicted to opioids. They’ve just swapped their opioid of choice for a slightly less damaging opioid. Now, this is an important step in recovery, because it makes further treatment and behavioral therapy possible. Suboxone’s high is there, but it isn’t the same rush as other opioids, so you maintain a sense of normalcy, rather than the altered state you get with heroin or stronger prescriptions. But the goal of taking suboxone is not to take it forever, but to use it as a temporary crutch, then rehabilitate to the point where you no longer need any substances. That is a long, difficult road, but it is the ultimate goal of true recovery. Using Suboxone is a part of that journey, but it is not the destination. Still, a number of people who find themselves using suboxone never find themselves moving on to the next step. For them, suboxone becomes like a treatment for a chronic illness, rather than a treatment that help them beat the illness. Of course, it’s true that addiction never completely goes away, but it can be beat back into remission with consistent effort and proper treatment. So what happens when the recovery process stops at suboxone? Is it okay to end up perpetually taking suboxone? What are the long-term effects of suboxone, and what are the pros and cons?
“Get the help you need today. We offer outpatient assistance, so you can maintain your work, family, and life commitments while getting the help you deserve!”
The Pros of Long-term Suboxone Use
The biggest pro of long-term suboxone use is simple: You’re not taking the (presumably more harmful) opioid you got addicted to in the first place. In that sense, at least, suboxone use is a successful outcome. Life on suboxone can definitely regain a feeling of normalcy. It will probably feel like you’ve beaten your addiction, since you’ve kicked the habit of your substance. You will regain control of your life to an extent, because suboxone’s effects aren’t as mind-altering as that of its more destructive cousins. There is no question that living with suboxone use is better than living with a full-on opioid addiction. If the choice is simply between those two outcomes, then suboxone is certainly a better option. And indeed, many people who struggle to kick their addictions end up on suboxone long-term simply because they find it to be “good enough,” and because the next step is so difficult. Realistically, there are many people who fall right back into their opioid addictions after stopping the use of suboxone. Worse still, since they’re used to a diminished dose of opioid agonists, they may try to go right back to dosage levels they were accustomed to before they started recovery. Because bodies build up a tolerance to opioids over time, and suboxone helps reduce that tolerance, a return to the same dosage as before is a recipe for a potentially fatal overdose. Suboxone is technically an opioid, and as such it can be used as a painkiller. But because of the unique blend of suboxone – an opioid antagonist and a partial agonist – the odds of suboxone abuse are much lower than they are for other opioids. Suboxone can still be addictive, but the cravings aren’t as strong as they would be for, say, OxyContin or heroin. 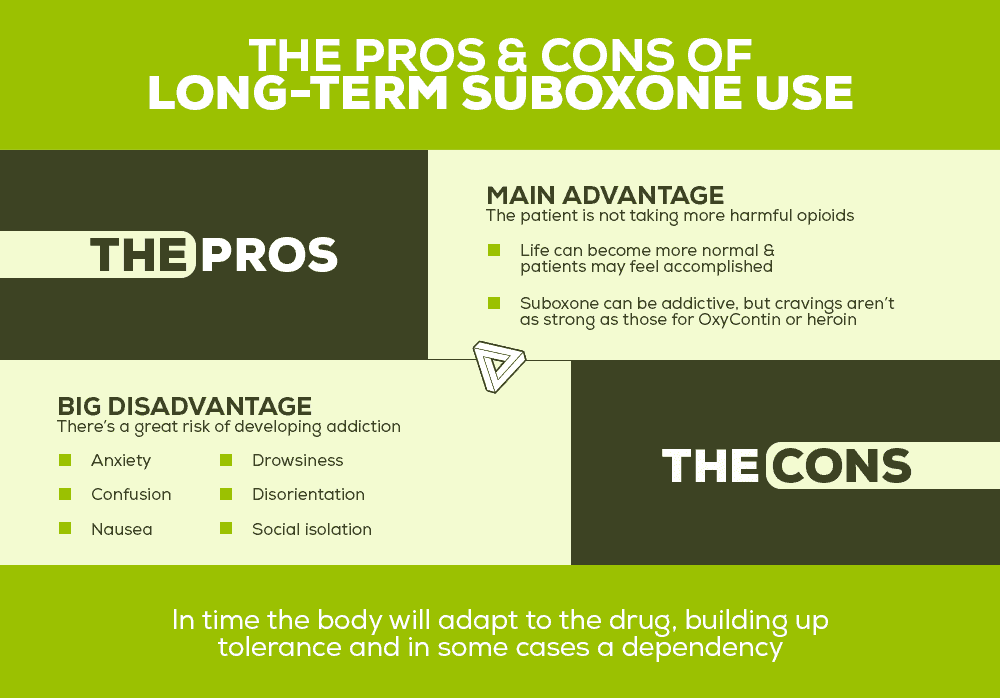
The Cons of Long-term Suboxone Use
The goal of substance abuse recovery isn’t to swap an addiction to one substance for an addiction to a not-as-bad substance. We don’t consider it a success if you enter our facility with an opioid addiction and leave as an alcoholic. In fact, we make it a point to look out for cross-addictions like that. This may sound strange to say, because people who are addicted to suboxone don’t have the appearance of an “addict.” Someone taking suboxone is taking it because they’re trying to recover. And there’s nothing wrong with that. But it’s a bad idea to get complacent with Suboxone use as a final solution. It is still an opioid, you can still get addicted, and you will build up a tolerance to it, same as any other opioid. In fact, long-term suboxone use has some very serious side effects, such as:
- Drowsiness
- Depression
- Anxiety
- Confusion/disorientation
- Constipation
- Social isolation
- Nausea/vomiting
- Decreased tolerance for pain
And these are just some physical and mental effects of long-term suboxone use. That’s to say nothing of the problems that are common to all forms of addiction, like a diminished sense of personal responsibility, damage to personal relationships, financial problems, and potential legal issues. The debate surrounding suboxone as a simple detox drug or a long-term solution continues in the medical community, and likely will for the foreseeable future. There are tradeoffs in both situations – shorter suboxone use means a higher chance of relapse, while extended suboxone use can be habit-forming on its own. In addition, suboxone, being as it is a potentially habit-forming opioid, has withdrawal symptoms of itself to deal with. 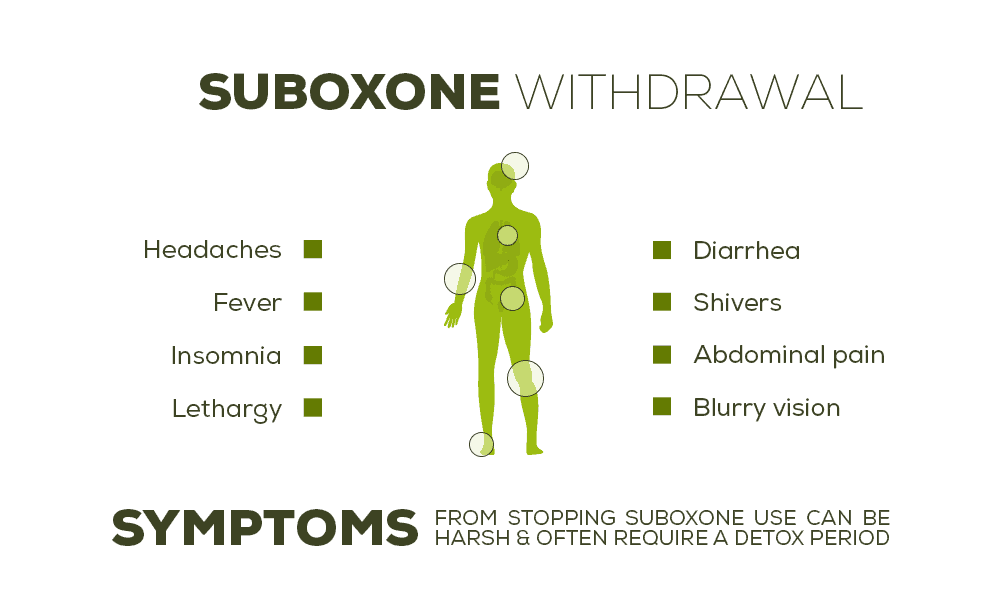
Suboxone Withdrawals – Detoxing from the Detox Drug
It’s a sad truth, but it’s true. Suboxone is often administered during medical detoxification from opioids, but in many cases, it comes with its own set of withdrawals. That’s right, it’s entirely possible that you may need to detox from the drug you get for detox. That may seem counter-intuitive, but it’s exactly why suboxone is not a good option for long-term addiction treatment. It truly should be a stepping stone for total sobriety, not a plateau at which the recovery process stops. The longer you stay on suboxone, the more your body adapts to it, and the greater the odds you’ll have a difficult time getting off of it. People who suffer from suboxone withdrawals may experience symptoms like:
- nausea/vomiting
- headaches
- digestive problems
- anxiety
- depression
- irritability
- muscle aches
- insomnia
- lethargy
- fever/chills
- headaches
Many of these symptoms are similar to the side effects of long-term suboxone use. And while it’s true that even the best medications can have side effects like these, this is just further proof that suboxone isn’t a harmless thing to take in the long term. Because the withdrawal symptoms from suboxone can be significant, it often requires a detox period. Which means yes, you will have to detox from the detox drug. And in many cases, the detox from suboxone is even more difficult than the initial opioid detox.
“We accept many health insurance plans. You can get your life back in order with our outpatient program today!”
The reason for this is twofold. First off, when you detox from opioids, suboxone is the substance that helps to lessen those withdrawal symptoms. But when you detox from suboxone, there is no “step-down” substance. In many ways, suboxone tends to just delay the inevitable. When you detox from suboxone, you’re still just detoxing from opioids. But because of the extended-release nature of suboxone, it is a more stable substance that takes much longer to flush out of the system. As a result, suboxone detox can be even more difficult than other opioid detox processes, and can take up to a month of sleeplessness, anxiety, and pain. This is a big part of the reason it is important to move on from suboxone before it takes root in addiction.
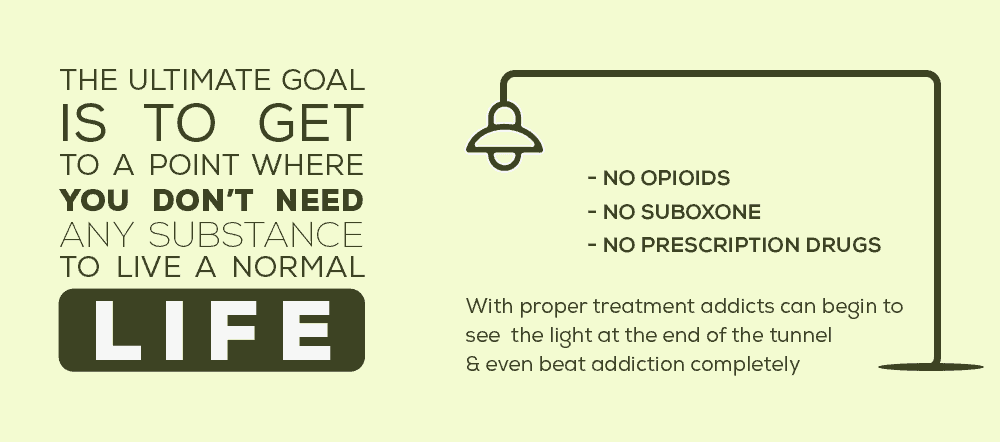
Using Suboxone on the Way to a Full Recovery
But if your goal is to get completely sober, the path to take is clear. While suboxone can be a useful drug to help detox and kick-start the recovery process, the ultimate goal is to get back to a point where you don’t need any substance to live a normal life. That means no prescription drugs, no heroin, no suboxone. If you go through proper addiction treatment, you can see the light at the end of that tunnel, where you don’t have to settle for “good enough” but can go right on past that to beating addiction entirely. Ultimately, suboxone is a great help to people who have nowhere else to turn. But its greatest benefit is in helping people be receptive to real addiction treatment. When you suffer from addiction, the substance or process that caused the addiction is only secondary. The reason it’s so easy to move from one addiction to another is because addiction itself is the problem. Once you become addicted, your mental processes change, and you become more prone to compulsive behaviors in the future. This is why suboxone alone will not make you overcome addiction. It can release you from the grip of your particular substance of choice, but until you truly understand the nature of your addiction and develop strategies for recognizing and avoiding compulsive behavior in the future, you will not have truly overcome your addiction. Luckily, suboxone exists as a great way to bring you back from the brink and make you much more receptive to the real addiction treatment you need. But it is, ultimately, a painkiller. Like any painkiller, it treats the uncomfortable symptom, not the problem. Addiction is the problem. Opioids are the symptom. To truly get your life back, you have to treat both, and with the right treatment and persistence, you will.
What Did you Think About This Blog?
Give it a Rating!