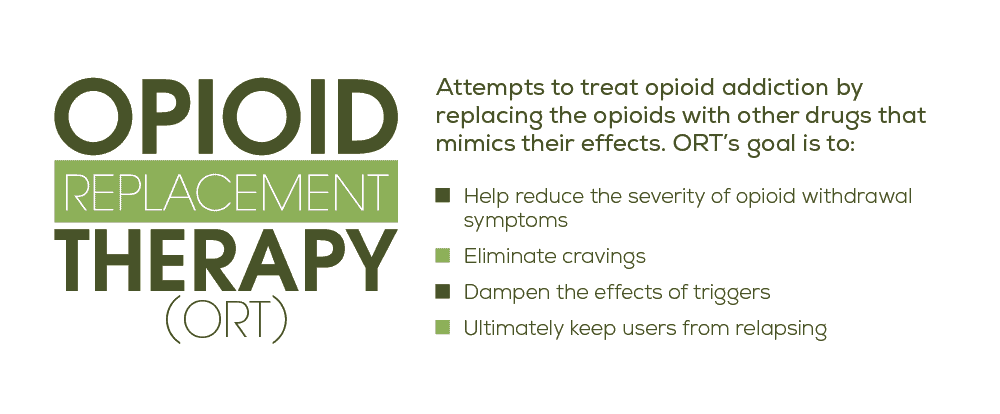
ORT or Opiate replacement therapy is becoming more widely used by medical professionals with each passing year. These medications not only help reduce the severity of the crippling symptoms of opioid withdrawal, but they can also eliminate cravings, dampen the effects of triggers, and ultimately keep users from relapsing. This method of using ORTs to help treat addiction (rather than therapy itself) is one benefit of learning to look at addiction as an actual disease and is integral to long-term recovery. We’ll get into the specifics of how these drugs can be instrumental in treating opioid dependence soon. But first, let’s take a minute to talk about how opiates work in the first place to make understanding ORTs even easier.
“Get the help you need today. We offer outpatient assistance, so you can maintain your work, family, and life commitments while getting the help you deserve!”
Opiates and the Body: A Closer Look
The brain is made up of a vast array of different cells. Some of these cells (called receptors) specialize in detecting and mingling with specific chemicals or neurotransmitters. Here’s how it works: each neurotransmitter has a unique physical shape that fits perfectly into its matching receptor. When a specific neurotransmitter bumps into it, then, it gets locked in place. This, in turn, sets off a chain reaction that can end up producing a variety of effects in the body, one of which could be the release of dopamine. Dopamine is incredibly useful for us as it’s the body’s natural reward chemical. Everything you can think of that produces pleasure (whether it’s reading a good book, eating a great meal, or even having sex) causes the brain to release dopamine. How opioids work is they hijack these receptors and activate them because they have a matching physical structure. As a result, they cause the release of dopamine, but up to 10 times more than your body naturally produces, making them highly addictive.
A Brief Overview of Opioid Addiction
Opiate addiction is one of the fastest growing substance use disorders in the world. The CDC reports that since 1999, overdose deaths involving opioids have risen by over 400%. The problem has gotten so bad that it’s now labeled by many government agencies as an official epidemic. Part of what makes opioids so addictive is the fact that they have such a powerful effect on the body. Pain relief and sedation are two of the main effects but abusing opiates can also cause intense euphoria as well. What’s more, many people find themselves accidentally becoming addicted to opioids after taking prescription pain relievers. In fact, research has shown that three out of four heroin users reported abusing such prescription drugs before turning to heroin.
Opioid Withdrawals
Another contributing factor to the growing opioid epidemic is the fact that coming off of an opiate addiction can be incredibly difficult. As the body acclimates to an opioid-free system, it experiences a wide range of uncomfortable side effects known as withdrawal symptoms. According to MedlinePlus, these symptoms include:
- Muscle aches
- Sweating
- Agitation
- Anxiety
- Insomnia
- Cramping
- Nausea
- Vomiting
- Diarrhea
And although going through opiate withdrawals isn’t fatal, the intensity of these symptoms can be unbearable. Many users end up turning back to using just to avoid having to experience such symptoms any longer. It’s clear, then, that finding new and more effective opiate addiction treatment options to reduce these effects should be a major focus when it comes to combating this spreading epidemic.
“We treat both addiction and co-occurring disorders and accept many health insurance plans. Take a look at our outpatient program today!”
What is Opiate Replacement Therapy?
Researchers have found that one of the best ways to reduce the chances of relapse is by using opioid replacement therapies during the recovery process. This type of therapy, also known as ORT, involves slowly taking you off of opioids by replacing the abused substance with a milder, less addictive opiate. The result is a much milder withdrawal that makes detoxing from opiates significantly more tolerable.
The Best Opioid Replacement Medications on The Market Today
While the majority of these opiate replacement prescriptions are used in ORTs today, they each have their own pros and cons as well as their own unique applications. And although the list below may point out the most notable characteristics, each of these should only be used under the guidance of a qualified professional. The success of any opiate replacement therapy relies on using these drugs carefully and appropriately whether it be in an inpatient or outpatient treatment center. What’s more, taking any of these opioid addiction treatment medications without proper medical guidance may be life threatening. So don’t risk it: consult a physician first. And of course, all of these medications are meant to be just one part of a well-rounded treatment plan that include therapies like CBT, DBT, and more.
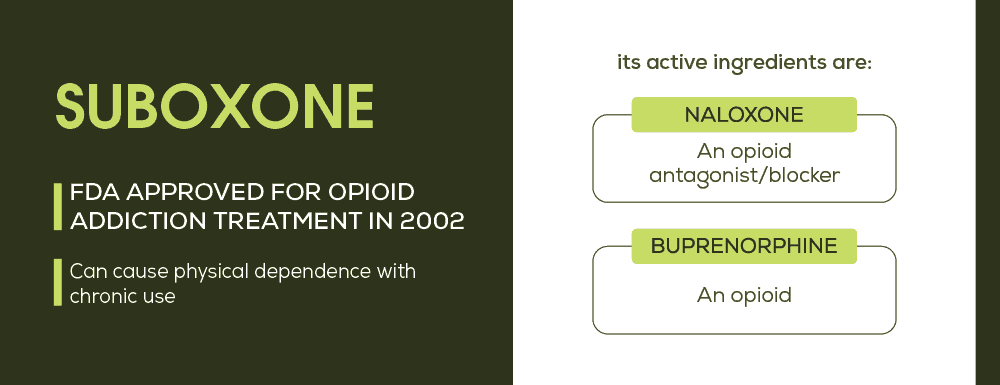
Suboxone for Opiate Replacement Therapy
Suboxone is by far the poster boy of opioid replacement therapies. In fact, when it was first approved to treat opioid addiction by the FDA in 2002, many physicians considered this opioid replacement medication to be a wonder drug. Besides its effectiveness in helping opioid addicts persevere through the stages of withdrawal, its main component (buprenorphine) was the first opioid dependency medication that could be prescribed and dispensed at a doctor’s office rather than opiate addiction treatment centers, making it much more accessible. And it’s true, Suboxone can be instrumental in tackling opioid addiction. But as with many other drugs, it can, in fact, become a substance of abuse. As such, only qualified physicians that have undergone extensive training can prescribe Suboxone. What’s more, each doctor can only prescribe Suboxone to a limited number of patients as well – a measure in place to combat abusing the drug.
What Makes Suboxone So Special?
Suboxone is a combination of two unique chemicals that each play an important role in the viability of the drug in opiate replacement therapies. Buprenorphine, the main chemical behind Suboxone, is a partial opioid agonist. That means that instead of fitting perfectly into the opioid receptors like other opiates (agonists), buprenorphine is a partial fit. As a result, this chemical can stop the symptoms of withdrawal without causing a high. The naloxone part of Suboxone is meant to prevent its abuse. If Suboxone is melted and injected, the naloxone immediately causes the painful symptoms of opiate withdrawal. When Suboxone is taken properly though, it has no effect, making it a perfect deterrent for abuse.
“We accept many health insurance plans. You can get your life back in order with our outpatient program today!”
Suboxone Research Studies
Study after study has shown that the success rate of Suboxone treatment is far superior to many other drug replacement programs and treatment methods. One study conducted by the National Institutes of Health showed that patients were almost 6 times more likely to reduce their prescription painkiller abuse with Suboxone than without it. Extended Suboxone treatment has also been associated with substantial improvements for opioid-addicted young adults and is more effective than methadone in treating neonatal abstinence syndrome (NAS).
The Downside of Suboxone
As with any drug, there are a variety of Suboxone maintenance pros and cons. One downside is that Suboxone can in fact lead to physical dependence when used improperly. And just like other dependencies, a buprenorphine addiction isn’t pretty. Research also shows that buprenorphine is most effective when it’s used as a long-term maintenance plan rather than as a tapering therapy. And while some plans can last for just a few months, others might end up being much longer. Unfortunately, that means that some opioid addicts may have to stay on Suboxone maintenance for life. As such, one of the long-term effects of Suboxone use is a risk of developing a new physical dependency in place of the old one.
Precipitated Withdrawal: A Quick Side Note
With some opioid replacement medications, the threat of a state known as precipitated withdrawal is something to be aware of for recovering opioid addicts. As the name implies, this is when the body is in a sense launched into the state of withdrawal rather than eased into it slowly. As you know, opiates interact with your body by matching up with their respective receptors. They fit in the gap and cause a flurry of chemical and electrical activities that eventually lead to the effects of euphoria, pain relief, and slowed respiration. With certain opioid replacement medications, the opiates are kicked out of these receptors and replaced entirely. It could be by a partial agonist like buprenorphine or, as we’ll see, by an antagonist like naltrexone or an inverse agonist like naloxone. The removal of opioids from the receptors through artificial means (as with these substances) can spur on withdrawal almost immediately. That’s why many doctors follow the COWS protocol for opiate withdrawal, a scale that helps them determine when it’s safe to administer such substances. As such, it’s important that you follow the guidance of a medical professional during opioid replacement therapy. Not finding a proper rehab center may just hurl you head first into the very symptoms you were trying to avoid in the first place.
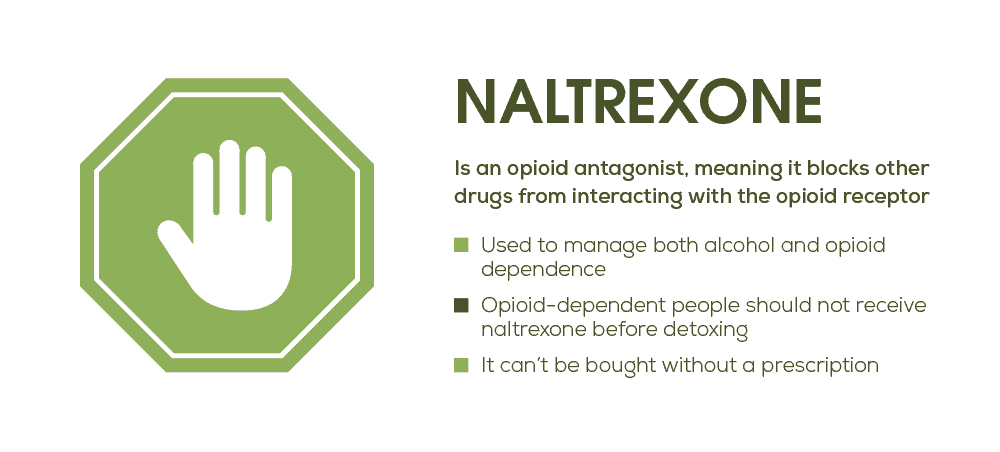
ReVia and Vivitrol
Two other popular drugs used in ORTs are ReVia and Vivitrol. ReVia is an opioid replacement prescription that comes in the form of a 50 mg tablet that is taken orally once a day while Vivitrol is administered by injection. This injection is 380 mg but is extended release and is only given once a month. Both of these drugs are made from the chemical naltrexone and can be extremely useful during opioid rehabilitation for two main reasons: it reduces cravings and is a way to remove the incentive of using again.
How Naltrexone Works
To explain, naltrexone is an opioid antagonist. That means that rather than activating your brain’s opiate receptors, this chemical actually blocks opioids from interacting with these receptors entirely. That means that no matter how much of an opioid you take, if you have enough naltrexone in your system then you won’t feel any of the favorable effects of the drug. It’s essentially a roadblock for your opiate abuse. The benefit here is, of course, that a moment of weakness won’t necessarily send you spiraling back into full-fledged addiction if you have ReVia or Vivitrol on your side. What’s more, the Substance Abuse and Mental Health Services Administration (SAMHSA) reports that research has shown that naltrexone actually decreases the severity of triggers as well.
Other Benefits of Naltrexone
There are a few other factors that make products like ReVia and Vivitrol such important opioid replacement medications when it comes to ORTs. The first is that naltrexone is not a true opioid replacement in that it isn’t an opioid agonist. This is an important point for some as there is now (and has been for years) a debate about whether it’s ethical to treat addiction with another addictive substance. Opiate replacement medications like methadone and buprenorphine, for example, are in fact active opiates. And for some people, organizations, and even countries (like Russia) treating addiction this way is immoral and even illegal. Naltrexone, then, is one way to help treat opioid addiction in places where such treatments are unavailable. And beyond that, naltrexone can be administered by any licensed physician. There are no special federal qualifications like with buprenorphine or treatment centers like with morphine.
What to Watch Out for With Naltrexone
As with any drug, it’s critical that you follow your doctor’s orders when taking naltrexone and that you’re completely honest with them about your drug habits. Many doctors will only prescribe ReVia or Vivitrol 7 to 10 days after full detoxification from opiates and if you aren’t truthful, you may risk precipitated withdrawal. Another downside is that this opioid addiction treatment medication may lower your opiate tolerance. As such, a relapse will not only fail to produce a high (because of the antagonist), it may also increase the risk of overdose and potentially death. And finally, naltrexone can’t be used with other opiate replacement medications. As an antagonist, it blocks off the receptors entirely. That means that while it can reduce the incentive of using again, it can’t do anything about the uncomfortable symptoms of withdrawal.
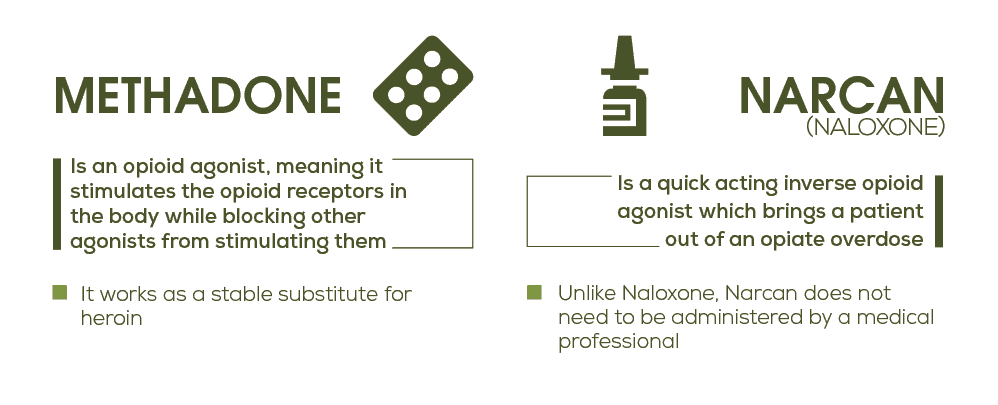
What is Methadone Replacement Therapy?
Methadone is one of the most tried and trusted opioid replacement therapies around. Its long and complex history began with its use as an analgesic and in 1972, it was first approved as a treatment for opioid dependency. An opioid agonist itself, the effects of methadone are long-acting and subdued but still may produce a slight sense of euphoria. Most importantly though, methadone can be one of the most helpful medications for drug addiction because it can help stave off symptoms of withdrawal. This point is absolutely crucial in that these symptoms are some of the main contributors to eventual relapse.
What Makes Methadone Different?
When compared to other opiate addiction treatment options, methadone usually comes out ahead as the most effective treatment, even more so than buprenorphine. One large-scale study even found that the difference between the success rates of the two could be as much as 10%. The main reason for this difference in effectiveness is that methadone has been around for much longer than buprenorphine. That extra time on the market has led it to be researched more and better understood. As such, doctors can prescribe it much more effectively. It’s also cheaper than other treatment methods and only needs to be taken once a day, two things that make recovery even more likely.
Cons of Methadone
One of the biggest flaws of methadone as an opioid replacement therapy is that it needs to be administered by specialized opiate addiction treatment centers. While this is absolutely necessary due to the inherent risk of addiction in methadone, it makes it harder to find treatment for some individuals. Beyond that, methadone can also be taken with other substances like alcohol to produce a high. This, of course, can make it harder for individuals to fully recover and may lead to years of continued methadone treatment.
Naloxone/Narcan in ORT
Not to be confused with naltrexone, naloxone is an inverse opioid agonist. While the exact method behind it is still up for debate, an inverse opioid agonist attaches to a receptor but causes the reverse effect as other opioids. As such, naloxone is primarily used to reverse the effects of opioid overdose which include:
- Loss of consciousness
- Very slow and shallow breathing
- Dangerously slow heartbeat
Up until recently, naloxone was administered by injection, a method which could take quite a while before becoming effective in the body. But during an overdose, every single minute counts. That’s why the development and distribution of Narcan is such a big deal in the addiction field. Not only does this method of naltrexone delivery work within about 5 minutes, it also comes in the incredibly easy-to-use form of a nasal spray. The benefit here is that practically anyone can administer this lifesaving medication, not just a qualified medical professional. In fact, using the drug is so easy and safe that free doses of Narcan are being sent to colleges around the country to help prevent as many overdoses as possible. And while it isn’t technically an opiate replacement therapy by itself, it has become an integral part of every opioid dependence treatment program. What’s more, it’s also a secondary chemical in Suboxone (discussed above) that prevents it from being abused as well.
Using Subutex for Opiate Replacement Therapy
Subutex is another type of ORT that utilizes the partial opioid agonist power of buprenorphine. Similar to Suboxone, it can be used to help stave off the uncomfortable symptoms of opioid withdrawal to help make full recovery more likely. However, Subutex has a significantly higher likelihood of abuse because it’s much easier to get high on it. The reason? Subutex doesn’t have the added chemical naloxone. Without it, abusers can melt down the Subutex film and use it intravenously for an opioid buzz. As such, many physicians have moved away from prescribing Subutex altogether.
GABA Mimicking Opioid Replacement Prescriptions
New research is emerging that shows that GABA emulators like baclofen and gabapentin (brand name Neurontin) may be effective methods for combating the unbearable symptoms of withdrawal in opiate addicts. These drugs also have been shown to help to curb the release of opioid-induced dopamine release. This is particularly beneficial because it cuts off the pleasure chemical that serves as the reward for drug-seeking behavior.
ORTs: The Smarter Way to Quit
There are an exceptionally wide variety of opiate replacement medications on the market today, each with their own specific benefits and detriments. And while the research overwhelmingly shows that like other medication assisted therapies, using opioid replacement medications during recovery leads to a higher rate of recovery, it should only ever be done under the guidance of a qualified medical professional. Simply put: it’s the smarter way to quit.
What Did you Think About This Blog?
Give it a Rating!